The Pharmaceuticalization of Marijuana
This article has been re-posted from the July – August 2003 Cannabis Health Journal.
By Dr. Lester Grinspoon
The government of the United States has a problem where medical marijuana is concerned. While there are many thousands of patients in the United States who currently use cannabis as a medicine, only seven are allowed to use it legally by the federal government. They are the survivors of the several dozen patients who were awarded Compassionate Use INDs during a period of time (from 1976 until 1991) when the government half-heartedly acknowledged that marijuana has medicinal properties.
This program was discontinued because of the exponentially growing numbers of Compassionate IND applications; the official reason was provided by James O. Mason, then chief of the Public Health Service: “It gives a bad signal. I don’t mind doing that, if there is no other way of helping these people… But there is not a shred of evidence that smoking marijuana assists a person with AIDS”. Each of the surviving IND recipients receives monthly a tin containing enough rolled marijuana joints to treat his or her symptoms for that month. Because the quality of the cannabis is poor, it requires more inhalation than a superior quality medicinal cannabis would. In fact, some of the recipients have been known to supplement this Government Issue with better quality street marijuana.
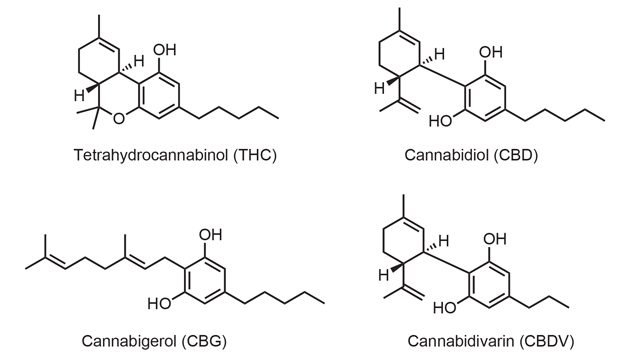
Because of increasing pressure from the many patients who find cannabis useful for the treatment of a variety of symptoms and syndromes, and the passage of Proposition 215 in California in 1996, the U.S. government funded the Institute of Medicine of the National Academy of Science to study the question of cannabis’ utility as a medicine. Its report, “Marijuana and Medicine: Assessing the Science Base” (published in 1999) timidly acknowledged that cannabis does indeed have therapeutic value. The growing understanding that cannabis is useful as a medicine presents a problem to the United States government: how can it make it possible for people who need it as a medicine to have unfettered access to marijuana, while at the same time prohibiting it to people who wish to use it for purposes the government does not approve of. A possible solution to this problem might be found in the “pharmaceuticalization” of cannabis: the development of prescribable isolated individual cannabinoids, synthetic cannabinoids, and cannabinoid analogs.
The IOM Report states that “…if there is any future for marijuana as a medicine, it lies in its isolated components, the cannabinoids and their derivatives.” It goes on:“therefore, the purpose of clinical trials of smoked marijuana would not be to develop marijuana as a licensed drug, but such trials could be a first step towards the development of rapid-onset, non-smoked cannabinoid delivery systems.”
Actually, the first attempt at pharmaceuticalization occurred in 1985 when the Food and Drug Administration (FDA) approved dronabinol (Marinol) for the treatment of the nausea and vomiting of cancer chemotherapy. Dronabinol is a solution of synthetic tetrahydrocannabinol in sesame oil (the sesame oil is meant to protect against the possibility that the contents of the capsule could be smoked). Dronabinol was developed by Unimed Pharmaceuticals Inc. with a great deal of financial support from the United States government.
This was the first hint that the “pharmaceuticalization” of cannabis might be what the government hoped would solve its problem with marijuana as medicine, the problem of how to make the medicinal properties of cannabis (insofar as the government believes such properties exist) widely available, while at the same time prohibiting its use for any other purpose.
But Marinol did not displace marijuana as “the treatment of choice”; most patients found the herb itself much more useful than dronabinol in the treatment of the nausea and vomiting of cancer chemotherapy. In 1992, the treatment of the AIDS wasting syndrome was added to dronabinol’s labeled uses. Again, patients reported that it was inferior to smoked marijuana. Marinol has not solved the marijuana-as-a-medicine problem, because so few of the patients who have discovered the therapeutic usefulness of marijuana use dronabinol. In general, they find it less effective than smoked marijuana, it cannot be titrated because it has to be taken orally, it takes at least an hour for the therapeutic effect to manifest itself and even with the prohibition tariff on street marijuana, Marinol is more expensive.
Thus, the first attempt at pharmaceuticalization proved not to be the answer. In practice, for many patients who use marijuana as a medicine the doctor prescribed. Marinol serves primarily as a cover from the threat of the growing ubiquity of urine tests.Some cannabinoid analogs may indeed have advantages over whole smoked or ingested marijuana in limited circumstances. For example, cannabidiol may be more effective as an anti-anxiety medicine and an anticonvulsant when it is not taken along with THC, which sometimes generates anxiety.Other cannabinoids and analogs may prove more useful than marijuana in some circumstances because they can be administered intravenously.
For example, 15 to 20% of patients lose consciousness after suffering a thrombotic or embolic stroke, and some people who suffer brain syndrome after a severe blow to the head become unconscious. The new analog dexanabinol (HU-211) has been shown to protect brain cells from damage when given immediately after the stroke or trauma; in these circumstances, it will be possible to give it intravenously to an unconscious person. Presumably, other analogs may offer related advantages.Some of these commercial products may also lack the psychoactive effects which make marijuana useful to some for nonmedical purposes.Therefore, they will not be defined as “abusable” drugs subject to the constraints of the Comprehensive Drug Abuse and Control Act.
Nasal sprays, vapourizers, nebulizers, skin patches, pills, and suppositories can be used to avoid exposure of the lungs to the particulate matter in marijuana smoke. The question is whether these developments will make marijuana itself medically obsolete. Surely many of these new products would be useful and safe enough for commercial development. It is uncertain, however, whether pharmaceutical companies will find them worth the enormous development costs. Some may be (for example, a cannabinoid inverse agonist that reduces appetite might be highly lucrative), but for most specific symptoms, analogs or combinations of analogs are unlikely to be more useful than natural cannabis. Nor are they likely to have a significantly wider spectrum of therapeutic uses, since the natural product contains the compounds (and synergistic combinations of compounds) from which they are derived. For example, the naturally occurring THC and cannabidiol of marijuana, as well as dexanabinol, protect brain cells after a stroke or traumatic injury.
The cannabinoids in whole marijuana can be separated from the burnt plant products (which comprise the smoke) by vapourization devices that will be inexpensive when manufactured in large numbers. These devices take advantage of the fact that finely chopped marijuana releases the cannabinoids by vapourization when air flowing through the marijuana is held within a fairly large temperature window below the ignition temperature of the plant material. Inhalation is a highly effective means of delivery, and faster means will not be available for analogs (except in a few situations such as parenteral injection in a patient who is unconscious or suffering from pulmonary impairment). It is the rapidity of the response to inhaled marijuana which makes it possible for patients to titrate the dose so precisely. Furthermore, any new analog will have to have an acceptable therapeutic ratio.The therapeutic ratio (an index of the drug’s safety) of marijuana is not known, because it has never caused an overdose death, but it is estimated, on the basis of extrapolation from animal data, to be an almost unheard of 20,000 to 40,000. The therapeutic ratio of a new analog is unlikely to be higher than that; in fact, new analogs may be much less safe than smoked marijuana, because it will be physically possible to ingest more of them. And there is the problem of classification under the Comprehensive Drug Abuse and Control Act for analogs with psychoactive effects. The more restrictive the classification of a drug, the less likely drug companies are to develop it and physicians to prescribe it. Recognizing this economic fact of life, Unimed Pharmaceuticals Inc. has fairly recently succeeded in getting Marinol (dronabinol) reclassified from Schedule 2 to Schedule 3.
Nevertheless, many physicians will continue to avoid prescribing it for fear of the drug enforcement authorities.
Now that the federal government has embarked on a cruel and so far successful campaign to close down buyers’ clubs, what options are available to the many thousands of patients who find cannabis of great importance, even essential, to the maintenance of their health? They can either use Marinol, which most find unsatisfactory, or they can break the law and use marijuana. Why is a government, which considers itself compassionate (“compassionate conservatism”), criminalizing these patients? What is the government’s problem with medical marijuana? The problem, as seen through the eyes of the government, is the belief that, as growing numbers of people observe relatives and friends using marijuana as a medicine, they will come to understand that this is a drug which does not conform to the description the government has been pushing for years. They will first come to appreciate what a remarkable medicine it really is; it is less toxic than almost any other medicine in the pharmacopoeia; it is, like aspirin, remarkably versatile; and it is less expensive than the conventional medicines it displaces.They will then begin to wonder if there are any properties of this drug which justify denying it to people who wish to use it for any reason, let alone arresting more than 700,000 citizens annually.
The federal government sees the acceptance of marijuana as a medicine as the gateway to catastrophe, the repeal of its prohibition. Insofar as the government views as anathema any use of plant marijuana, it is difficult to imagine it accepting a legal arrangement that would allow for its use as a medicine, while at the same time vigorously pursuing a policy of prohibition for any other use.
A somewhat different approach to the pharmaceuticalization of cannabis is being taken by a British company, G.W. Pharmaceuticals. It is attempting to develop products and delivery systems which will skirt the two primary popular concerns about the use of marijuana as a medicine: the smoke and the psychoactive effects (the “high”). To avoid the need for smoking, G.W. Pharmaceuticals has developed an electronically controlled dispenser to deliver cannabis extracts sublingually in carefully controlled doses. The company expects its products (extracts of marijuana) to be effective therapeutically at doses too low to produce the psychoactive effects sought by recreational and other
users.
My clinical experience leads me to question whether this is possible in many, or even most, cases. The issue is complicated by tolerance to the psychoactive effects. Recreational users soon discover that the more often they use marijuana, the less “high” they experience. A patient who smokes cannabis frequently for the relief of, say, chronic pain or elevated intraocular pressure will experience little or no “high”. Furthermore, as a clinician who has considerable experience with medical cannabis use, I have to question whether the psychoactive effect is always separable from the therapeutic. And I strongly question whether the psychoactive effects are necessarily undesirable. Many patients suffering from serious chronic illnesses report that cannabis generally improves their spirits. If they note psychoactive effects at all, they speak of a slight mood elevation – certainly nothing unwanted or incapacitating.
The great advantage of the administration of cannabis through the pulmonary system is the rapidity with which its effects are experienced.This in turn allows for the self-titration of dosage, the best way of adjusting individual dosage. With other routes of delivery the response time is longer and self-titration becomes more difficult. Thus, self-titration is not possible with oral ingestion of cannabis. While the response time for sublingual or oral mucosal administration of cannabis is shorter than it is with oral ingestion, it is significantly longer than that from absorption through the lungs and therefore a considerably less useful route of administration for self-titration.
Furthermore, the design of the G.W. Pharmaceuticals dispenser negates whatever self-titration capacity sublingual administration may have.The device has electronic controls that monitor the dose and prevent delivery if the patient tries to take more than the physician or pharmacist has set it to deliver during predetermined time windows. The proposal to use this cumbersome and expensive device apparently reflects a concern that patients cannot accurately titrate the therapeutic amount or a fear that they might take more than they need and experience some degree of “high” (always assuming, doubtfully, that the two can easily be separated, especially when cannabis is used infrequently).
Because these products will be considerably more expensive than natural marijuana, they will succeed only if patients are intimidated by the legal risks, and patients and physicians consider the health risks of smoking marijuana (with and without a vapourizer) much more compelling than is justified by either the medical or epidemiological literature and they believe that it is essential to avoid any hint of a psychoactive effect.
In the end, the commercial success of any psychoactive cannabinoid product will depend on how vigorously the prohibition against marijuana is enforced. It is safe to predict that new analogs and extracts will cost much more than whole smoked or ingested marijuana even at the inflated prices imposed by the prohibition tariff. I doubt that pharmaceutical companies would be interested in developing cannabinoid products if they had to compete with natural marijuana on a level playing field.The most common reason for using Marinol is the illegality of marijuana, and many patients choose to ignore the law for reasons of efficacy and cost. The number of arrests on marijuana charges has been steadily increasing and has now reached more than 700,000 annually, yet patients continue to use smoked cannabis as a medicine. I wonder whether any level of enforcement would compel enough compliance with the law to embolden drug companies to commit the many millions of dollars it would take to develop new cannabinoid products. Unimed is able to profit from the exorbitantly priced dronabinol only because the U.S. government underwrote much of the cost of development. Pharmaceutical companies will undoubtedly develop useful cannabinoid products, some of which may not be subject to the constraints of the Comprehensive Drug Abuse and Control Act.
But, it is unlikely that this pharmaceuticalization will displace natural marijuana for most medical purposes.
It is also clear that the realities of human need are incompatible with the demand for a legally enforceable distinction between medicine and all other uses of cannabis. Marijuana use simply does not conform to the conceptual boundaries established by twentieth century institutions. It enhances many pleasures and it has many potential medical uses, but even these two categories are not the only relevant ones.The kind of therapy often used to ease everyday discomforts does not fit any such scheme. In many cases, what lay people do in prescribing marijuana for themselves is not very different from what physicians do when they provide prescriptions for psychoactive or other drugs.
The only workable way of realizing the full potential of this remarkable substance, including its full medical potential, is to free it from the present dual set of regulations – those that control prescription drugs in general and the special criminal laws that control psychoactive substances. These mutually reinforcing laws established a set of social categories that strangle its uniquely multifaceted potential. The only way out is to cut the knot by giving marijuana the same status as alcohol – legalizing it for adults for all uses and removing it entirely from the medical and criminal control systems. Two powerful forces are now colliding: the growing acceptance of medical cannabis and the proscription against any use of the marijuana plant, medical or non-medical. There are no signs that the U.S. is moving away from absolute prohibition to a regulatory system that would allow responsible use of marijuana. As a result, we are going to have two distribution systems for medical cannabis: the conventional model of pharmacy-filled prescriptions for FDA-approved cannabinoid medicines, and a model closer to the distribution of alternative and herbal medicines. The only difference – an enormous one – will be the continued illegality of whole smoked or ingested marijuana. In any case, increasing medical use by either distribution pathway will inevitably make growing numbers of people familiar with cannabis and its derivatives. As they learn that its harmfulness has been greatly exaggerated and its usefulness underestimated, the pressure will increase for drastic change in the way we as a society deal with this drug.
____________________
Dr. Lester Grinspoon MD is an Associate Professor Emeritus of Psychiatry at Harvard Medical School. He has been studying cannabis since 1967 and has published two books on the subject: “Marihuana Reconsidered” (Harvard University Press, 1971) and “Marihuana, the Forbidden Medicine”, co- authored with James B. Bakalar (Yale University Press, 1993). He maintains two active websites: The Medical Marijuana website (www.Rxmarijuana.com) and The Uses of Marijuana website ( www.marijuana-uses.com).

